Blog
Shoulder Pain – Part 1
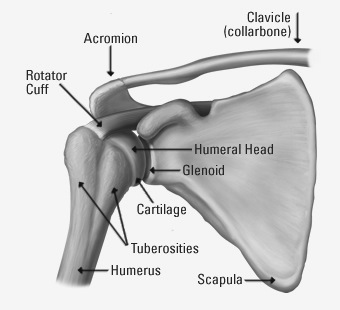
Diagram of the shoulder

The next two weeks, I’d like to address shoulder pain and injuries. Most people experience shoulder pain at some point in their lives. Doctors see it in athletes, people who overuse their shoulders, and others who may have fallen or received a blow directly to their shoulder, or fallen on their outstretched arm.
To understand shoulder pain, it’s important to know the basic anatomy of the shoulder joint itself (see diagram of the front of the right shoulder). The shoulder is one of the most complex joints in the body. Most joints permit a limited range of motion. The unique anatomy of the shoulder joint allows for a vast range of movements. It has to be relatively unstable compared to our other joints to be so versatile.
The easiest way to describe the shoulder joint is to picture a basketball sitting on a dinner plate. The basketball represents the head of the humerus, the spherical top part of the upper arm bone. The plate represents the glenoid, the part of the shoulder blade (scapula) that articulates with the head of the humerus. If you imagine the basketball sliding around on the plate, you can understand how unstable the shoulder joint is – the head of the humerus can slide around on the glenoid or even slide off the edge (dislocation).
There are anatomic structures that help reduce this instability. One is the glenoid labrum, a rim of cartilage that runs around the edge of the glenoid. It serves to shape it into more of a shallow bowl rather than a flat plate. The other structure is the rotator cuff, a juxtaposition of four tendons that attach around the head of the humerus to hold it in place. These four tendons are connected to four muscles that rotate the head of the humerus and help initiate arm movements. There are also fluid-filled bursa sacs around the joint that help cushion the movements of the tendons. As I said, it’s a complex joint!
Now that you’re an expert in anatomy, let’s examine what can go wrong. I don’t want to cover fractures since they are usually pretty obvious. I also don’t have enough space to cover all shoulder injuries, so I’ll need to finish up next week.
I’ll start with rotator cuff injuries. These are injuries to the tendons and/or muscles that make up the rotator cuff. These structures can be inflamed, stretched, partially torn, or completely torn. The injury may involve one or more of the four tendons.
Rotator cuff injuries usually happen when someone falls on an outstretched arm causing the humerus to act as a lever that puts excess force on the cuff tendons or their muscles. Cuff injuries can also occur when someone falls on an elbow that causes the head of the humerus to be forced out of its normal position in the glenoid. Other forces on the arm may cause the humerus to slide around on the dinner plate (subluxation) or completely slide off the dinner plate (dislocation), leading to cuff injuries. Finally, overusing one’s arm, such as when forcefully throwing, can stretch or tear the tendons.
Symptoms of rotator cuff injuries depend on the severity of the trauma and can be quite subtle. The shoulder may simply be achy. Some may notice severe pain when moving the shoulder in a particular direction, especially raising it in a forward or sideways direction. Others may note obvious weakness. Since the rotator cuff tendons are responsible for initiating arm movements, patients with tears may note they have trouble starting movements, especially raising the arm to the front or side.
Treatment of rotator cuff injuries depends on the type of injury as well as the age and activity level of the patient. The goal is to stabilize the joint as much as possible by rehabilitating the shoulder muscles to return the patient to maximum possible function. Young patients and athletes usually receive aggressive treatment including physical therapy and, if they have a torn tendon, often surgery. Elderly or less active patients often do fine with physical therapy alone to strengthen the cuff muscles in the shoulder.
Stay tuned next week when I’ll cover shoulder dislocations, impingement, and bursitis.
– Dr. John Roberts is a member of the Franciscan Physician Network specializing in Family Medicine.
