Blog
Heat Illness

Since our temperatures are predicted to be near 100 early this week, it’s time to start thinking about the dog days of summer. Although I don’t see a significant number of heat-related emergencies in my office, many patients suffering from heat illness will start filling the beds in emergency departments.
Heat illness accounts for tens of thousands of visits each year to doctors’ offices and emergency rooms. Deaths from heat-related illness in America range from 300 to several thousand per year. The number is increasing with our warming climate that is resulting in an increased number and intensity of heat waves (see the new records being set in the Southwest).
Risk factors that the predispose to heat-related illness include being elderly, very young, or obese. Certain prescription and non-prescription drugs including antihistamines, beta blockers, diuretics, ADD/ADHD medications, and some psychiatric medications increase the risk, as does alcohol. Workers like firefighters who must wear heavy clothing are at very high risk.
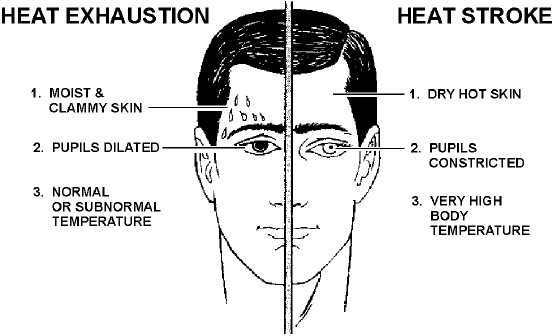
Absorbing too much heat from the environment or producing too much heat internally leads to heat illness. Heat exhaustion and heat stroke are the two main types of heat illness.
Heat exhaustion is caused by excessive loss of body water and electrolytes. Heat exhaustion typically comes on slowly and is characterized by fatigue, weakness, nausea, vomiting, headache, muscle aches, cramping, dizziness, and irritability. Victims are usually pale, sweating profusely, have clammy skin and a weak, rapid pulse. Low blood volume from dehydration results in reduced blood flow to the organs, known as circulatory shock.
The first thing to do for someone with heat exhaustion is to remove the person from the hot environment. Standard treatment for shock should then be administered. Elevating the legs above the level of the chest helps get blood to the vital organs and brain. Sports drinks such as Gatorade® or Powerade® are an excellent way to replace water and lost electrolytes.
If a victim shows signs of confusion or lethargy, or is not responding to treatment, rescuers should contact 911 or immediately take the victim to an emergency department. The prognosis for heat exhaustion is usually very good.
Heat Stroke is a different story. It results when the body’s temperature regulating mechanisms malfunction, causing an inability to transfer internal body heat to the environment. This can cause dangerously high internal body temperatures, sometimes as high as 105-106 ºF. Heat stroke is a medical emergency and is frequently fatal without immediate treatment.
Symptoms of heat stroke usually come on rapidly and include headache, dizziness, fatigue and weakness. Physical findings can include confusion, hot and dry skin, decreased sweating, rapid pulse, vomiting, loss of consciousness and sometimes seizures.
Heat stroke is a medical emergency and requires immediate medical care, typically a call to 911. While waiting for EMS to arrive, remove the person from the hot environment and place the person in a bathtub or other tub filled with very cold water, preferably with some ice. Emergency services will usually observe the patient on-site until his or her core temperature has dropped below 102-103 ºF. If a tub is not available, place ice packs over the armpits, groin, neck and abdomen to help cool the patient down. Running a fan on the patient and spraying them with cool water can also be very effective in lowering their temperature.
As with most potential serious medical problems, the key is prevention. When you’re in the sun or a hot environment for an extended period, be sure to maintain your hydration. Water will do just fine unless you’re involved in intense physical activity for more than an hour. If that’s the case, consider adding in sports drinks. Salt tablets are not recommended.
You should drink roughly 16 ounces of fluid about two hours before outdoor activity if possible. Drink 4 to 8 ounces every 20 minutes during activity. A crude measure of adequate hydration is the color of your urine – clear or pale yellow is what you’re aiming for.
Make sure young children and elderly family or friends stay out of the heat. Also make sure the elderly have a functioning cooling system in their home or apartment and that they have access to fluids.
If you take prescription medication, be sure and read the warnings you receive from the pharmacist or talk to your doctor to determine if it might affect your sensitivity to heat. If you develop any of the symptoms mentioned above, tell someone and get to a cool environment immediately.
Dr. John Roberts is a member of the Franciscan Physician Network specializing in Family Medicine.
