Blog
What Causes Shingles And What To Do About It
By: John Roberts
I’ve had a number of requests to re-run my column on shingles. This may be due to the successful marketing campaign for Shingrix® vaccine, developed to reduce the incidence of this often painful malady. The ads are quite accurate and compelling.
Shingles is a condition caused by the Varicella-Zoster Virus (VZV). The virus is also known as chickenpox virus, varicella virus, and zoster virus. It is one of eight types of herpes viruses that infect humans.
The biology of herpes viruses is very interesting. They infect humans through the skin and the mucus membranes that line body openings. The initial or “primary” VZV infection causes the typical chicken pox rash that develops shortly after exposure to the virus. This usually causes itching and redness of the skin followed by development of small fluid-filled blisters known as vesicles. Some older readers may have seen chicken pox, but virtually all of today’s parents have not. Thankfully, it is becoming a very rare condition since the introduction of the childhood varicella vaccination in the U.S. 1995.
Interestingly, herpes viruses are never completely cleared from the body. Once the initial infection has subsided, the viruses take refuge in collections of nerve cells called ganglia that reside deep in the body.
Shingles is a condition where VZV reactivates and begins to reproduce causing a recurrent outbreak. As the viruses begin to multiply, they migrate from the ganglia near the spinal cord and propagate along the nerve fibers of one or more (usually adjacent) spinal nerves to the surface of the skin.
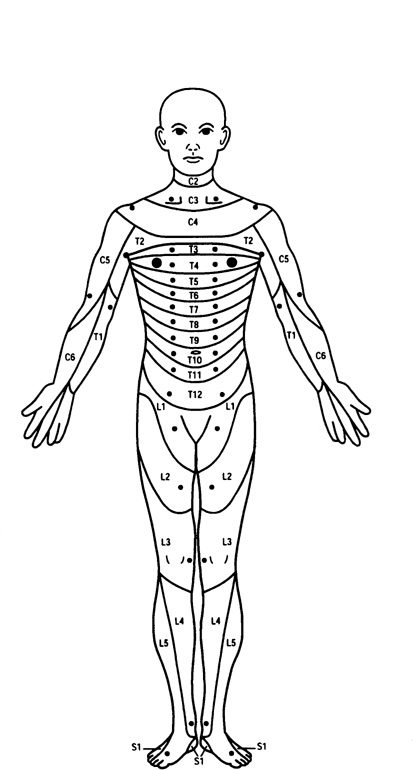
The appearance of the shingles rash can be explained by knowing a bit about the anatomy of the nervous system. The peripheral nervous system is made up of sensory and motor nerves that enter and exit the spinal cord in the neck and back. The sensory nerves carry nerve impulses for feeling (touch, pain, etc.) from specific bands of skin called dermatomes (see diagram). These sensory nerves enter the spinal cord at specific levels. Dermatomes stop at the midline of the body (i.e. there are right and left dermatomes supplying feeling at each level of the spinal cord).
When VZV reactivation occurs, the person usually feels some itching, burning or tingling along the involved dermatome(s). This is typically followed a day or two later by the formation of blistering skin and pain. The pain may precede the rash by a few days, sometimes fooling the patient and the doctor into thinking it’s something else. I have had patients thought the pain was from kidney stones who underwent expensive workups in the emergency room, only to develop the rash shortly after their visits.
It’s important to point out that Shingles almost always presents in a single dermatome on one side of the body. It rarely crosses the center of the body (there is no truth to the adage that a person with shingles will die if the rash crosses the center of the body).
The varicella virus can also affect the nerves that supply sensation to the eye, a condition called herpes zoster ophthalmicus. These infections can be quite severe and can lead to scarring of the front of the eye (cornea) that may require corneal transplantation. People with shingles on the tips of their noses often have involvement of the eye as well.
Shingles may last a week or two, sometimes longer. Unfortunately, about 15 percent of people, primarily seniors, develop severe pain that persists after the rash is gone. This condition is called post-herpetic neuralgia (PHN). It can be extremely devastating and may require potent medication to keep the pain tolerable. One of my friends has not found anything to help the pain he’s had for many years. He describes it as a “blowtorch” on his skin.
About a third of adults who have had a primary varicella infection will develop shingles. The main reason for developing a reactivation is reduced or waning immunity. Ninety-five percent of adults in the U.S. have antibodies to VZV. This is either through natural immunity from having had chicken pox as a child or from vaccine-associated immunity from receiving varicella vaccine.
As people age, their immune systems become weaker and they are less likely to be able to keep VZV in the resting stage. Other conditions such as infections or malignancies can also trigger an outbreak of shingles. Most cases of shingles are not the result of severe underlying problems.
It is important to see a physician as soon as you suspect you may have shingles. There are anti-viral medications available that slow the spread of VZV and can also greatly reduce the risk of developing PHN. To be most effective these medications should be started within 72 hours of the start of symptoms.
Since post-herpetic neuralgia can be so devastating, it is important for people over 50 years of age to consider vaccination against VZV with the Shingrix® vaccine. It is one of the most effective vaccines we have, offering up to 97% protection, even in the elderly. It is available in most doctors’ offices or pharmacies. Most insurance companies cover the cost of the vaccine. Beginning this year, the vaccine is covered for people who have a Medicare Part D plan or a Medicare Advantage plan. The vaccine is given in two doses, two to six months apart. Most people who have had severe shingles would be very quick to advise everyone to get vaccinated.
– Dr. John Roberts is a retired member of the Franciscan Physician Network specializing in Family Medicine.
